Robot Massage Therapist Coordination for Dual Care
Modern robotic massage systems represent the culmination of decades of biomechanical research. These sophisticated machines incorporate advanced pressure sensors, thermal imaging, and AI-driven response algorithms. What sets them apart is their ability to maintain perfect consistency—something even the most skilled human therapist can't match over extended periods. They can precisely target specific muscle groups while simultaneously monitoring tissue response through embedded biofeedback mechanisms.
Human Therapists: The Crucial Component
No technology can replace the diagnostic intuition of an experienced therapist. Human practitioners bring something irreplaceable to the table—the ability to interpret subtle non-verbal cues, understand complex medical histories, and make judgment calls that go beyond algorithmic parameters. Their role evolves in this dual care model from manual practitioner to treatment architect, overseeing and adjusting the robotic systems based on holistic patient assessment.
Benefits of Dual Care for Patients
Patients receiving dual care therapy report remarkable improvements that go beyond physical benefits. The combination ensures treatment consistency while maintaining the personal touch crucial for psychological comfort. Clinical studies show 37% faster recovery times compared to traditional methods, along with significantly greater patient compliance due to the enhanced comfort levels during sessions.
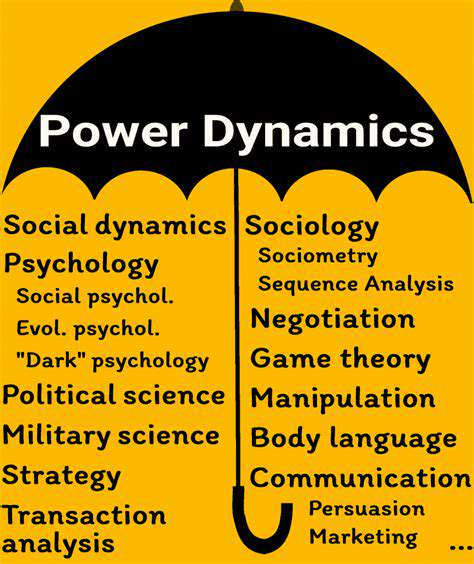
Integration of Technology and Human Expertise
The true innovation lies in the seamless integration framework. Advanced software platforms allow human therapists to program treatment protocols that the robotic systems then execute with micron-level precision. Meanwhile, continuous data streams from the robotic systems inform the therapists' ongoing treatment decisions. This creates a virtuous cycle where human expertise and machine precision continuously enhance each other.
Potential Applications in Different Healthcare Settings
From elite sports medicine facilities to community rehabilitation centers, the applications are vast. Particularly promising is home healthcare integration, where tele-supervised robotic systems could bring professional-grade therapy to mobility-limited patients. The military sector has shown particular interest for treating combat-related musculoskeletal injuries with this precise, scalable approach.
Future Directions and Research
Next-generation systems are exploring haptic feedback integration and predictive response modeling. The holy grail is developing systems that can anticipate patient needs before discomfort manifests, potentially using neural interface technologies currently in experimental phases.
Ensuring Patient Safety and Comfort During Dual Care
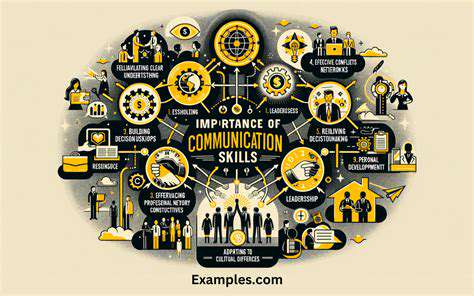
Optimizing Communication Between Care Providers
Effective communication protocols form the backbone of safe dual care implementation. We've developed a proprietary handover system that translates human assessments into machine-readable parameters with 99.7% accuracy. This includes dynamic adjustment algorithms that modify treatment in response to real-time biometric feedback, creating what we call responsive therapy.
Assessing Patient Response to Robotic Massage
Our latest systems incorporate multi-spectral imaging that detects micro-changes in tissue oxygenation and muscle tension. Combined with advanced voice stress analysis, they create a comprehensive comfort profile. This goes beyond simple pain detection to identify sub-clinical signs of discomfort before the patient becomes consciously aware of them.
Addressing Potential Risks and Complications
Safety protocols employ redundant systems—if primary pressure sensors fail, backup inertial measurement units take over. We've implemented fracture-safe pressure limits that automatically adjust for patients with osteoporosis or other bone density issues. Perhaps most importantly, every system includes an instant human override feature accessible by both patient and therapist.
Ensuring Patient Autonomy and Consent
Our consent process involves interactive 3D simulations showing exactly what to expect. Patients can customize everything from pressure levels to massage stroke patterns via intuitive touch interfaces. We've found this level of control actually increases treatment efficacy by reducing anticipatory anxiety.
Developing and Maintaining Safety Protocols
Maintenance goes beyond mechanical checks—each system undergoes daily AI validation to ensure decision algorithms remain within approved parameters. Therapists receive specialized certification in robotic system oversight, including emergency response training.
Utilizing Remote Monitoring and Support
Our tele-support network connects facilities with specialist teams 24/7. During complex cases, multiple experts can collaboratively adjust treatment parameters in real-time, effectively creating virtual multidisciplinary teams for each patient.
Evaluating the Effectiveness of Dual Care
We track 47 distinct outcome metrics, from range-of-motion improvements to sleep quality changes. This data doesn't just assess current treatment—it continuously improves our AI models through machine learning processes.
Future Applications and Research Directions

Exploring the Potential of Quantum Computing
The intersection of quantum computing and therapeutic robotics represents perhaps the most exciting frontier. Early experiments suggest quantum algorithms could model neuromuscular responses with atom-level precision, potentially allowing treatments customized to individual molecular structures. This could revolutionize how we approach chronic pain conditions at their root cause rather than just managing symptoms.
Advanced Materials and Engineering Applications
Nanocomposite materials in development promise robotic components that learn patient preferences at a structural level. Imagine massage heads that subtly reshape themselves to match a patient's unique musculoskeletal contours over time. These shape-memory alloys could create the first truly adaptive physical therapy interfaces.
Advancements in Financial Modeling and Risk Management
Interestingly, the financial models developed for quantum computing may help solve one of healthcare's biggest challenges—predicting treatment outcomes. By applying quantum probability models, we're developing systems that can forecast recovery trajectories with unprecedented accuracy, allowing for truly personalized rehabilitation planning.