Postpartum Depression’s Effect on Marriage and Recovery Tips
Index
1 in 7 women is affected by postpartum depression, and its impact extends far beyond the mother herself.
Postpartum depression is fundamentally different from baby blues and may last for months or even years without treatment.
Marital relationships face both communication barriers and emotional stress.
Open dialogue is an important emotional bond in coping with postpartum depression.
The family ecosystem may experience a chain reaction due to postpartum depression.
Family therapy can restore the parent-child relationship network impacted by depression.
Partner support requires a balance between concrete actions and self-care.
The timing of professional interventions directly affects recovery outcomes and processes.
Support groups provide genuine emotional resonance and practical wisdom.
Quality time alone as a couple is the emotional adhesive for repairing relationships.
Mental health conversations need to break social prejudices and stereotypes.
The authenticity of emotional expression determines the breakthrough potential of depression challenges.
Social stigma creates multiple barriers to seeking help.
Self-care mechanisms are foundational to mothers' psychological rebuilding.
Alternative therapies provide beneficial complementary options to traditional treatment.
The Emotional Cost of Postpartum Depression
Understanding This Invisible Trauma
Postpartum depression is like an invisible net that envelops about 14% of new mothers. Remember Ms. Li from our community last year? She always wore a tired smile while walking with her baby until one day she suddenly disappeared for two weeks—later we learned she was hospitalized for depression. This mental state is like a chameleon, manifesting as inexplicable irritability, a persistent feeling of emptiness, or a loss of interest in daily activities.
It is crucial to distinguish between short-term mood swings and clinical depression that requires professional intervention. Just like a cold and pneumonia both require treatment but to different degrees, postpartum mood disorders have significant differences. A psychologist friend told me that in her cases, the longest untreated depression lasted 22 months, which was a huge drain on the whole family.
Stress Testing the Marital Relationship
When a wife experiences postpartum depression, marriage is like a ship sailing in a storm. Mr. Zhang once confided in me that he felt like a clumsy mediator during that time: having to care for a crying baby while also soothing his emotionally unstable wife. Research shows that couples in such circumstances experience a 47% increase in quarrels and a reduction of about two-thirds in intimate behaviors.
A marriage therapist offered an interesting analogy: Communication during this time is like walking on a frozen lake, requiring special caution and skill. It is recommended to use an emotional thermometer method, evaluating each other’s state daily on a scale from 1 to 10 to establish a non-blaming communication mechanism.
The Chain Reaction of Family Ecology
Do you remember the little boy who always stared blankly in the corner of the playground? His mother later revealed that during her postpartum depression, she couldn’t establish an emotional connection with her child at all. Research published in the Journal of Emotional Disorders confirms that such early emotional deprivation may affect a child's social skills development by the age of 5-7. Like a domino effect, the mental health issues of one family member can trigger shocks to the entire family system.
A family therapist shared an effective method: set a time for emotional reboots. Every day, fix a 15-minute slot for the whole family to sit together and share the happiest moments of the day; this simple ritual can gradually repair damaged emotional connections.
Practical Strategies to Support Partners
Mr. Wang’s approach is worth emulating: he made support cards listing 20 specific tasks his wife might need help with, from helping her apply heat to her shoulders to taking the child for a one-hour walk. This visual support plan is much more actionable than vague offers to help.
Knowledge accumulation is equally important. One husband, after attending a postpartum care course, finally understood that his wife's sudden sensitivity to smells was not just a whim, but a physiological reaction caused by hormonal changes. This cognitive shift significantly alleviated the couple's conflicts.
Diverse Choices for Professional Intervention
A psychiatric department head from a top-tier hospital in Shanghai shared a typical case: using cognitive-behavioral therapy combined with light therapy shortened the patient’s recovery time by 40%. In terms of medication, new SSRIs have been confirmed safe for use during breastfeeding by multiple studies.
It is noteworthy that the value of support groups is often underestimated. A mutual aid group in Beijing, made up of recovering mothers, has developed a unique emotional journaling method that has helped over 300 families find their suitable recovery rhythms.
The Gradual Road to Couple Recovery
Mr. and Mrs. Liu have a creative micro-date plan: during their baby’s afternoon nap, they spend 20 minutes indulging in specially prepared snacks to maintain emotional connection. These fragmented moments of intimacy accumulate and are just as effective as formal dates.
One aspect that is often overlooked during recovery is the non-linear nature of progress. Just like tides ebb and flow, emotional recovery can be cyclical. Establishing a fallback emergency plan and pre-agreeing on responses when one partner's mood dips can effectively reduce feeling at a loss.
Long-term Perspectives and Social Cognition
A dad experience camp initiated in a community in Hangzhou is worth promoting: allowing husbands to wear pregnancy simulation devices to personally experience the discomfort caused by bodily changes. This immersive education has led to a deeper understanding of postpartum depression for 95% of participants.
Breaking stigma requires specific scenario breakthroughs. For example, increasing mental health assessment segments during prenatal check-ups and creating mental health info corners in maternity stores to translate professional terminologies into the everyday language of mothers.
Deconstructing Communication Barriers
The Shifts in Family Interaction Patterns
During postpartum depression, family communication often falls into an emotional telegram mode: brief, functional conversations replace deep exchanges. As Ms. Chen described: we were like two clumsy acrobats, so focused on not dropping the child that we forgot to connect through eye contact.
Research shows that the importance of non-verbal communication increases by 60% in such cases. Simple physical contact—like lightly touching each other’s arm while doing dishes—can maintain basic emotional connection. Some couples have even invented stress bracelets, where one partner's vibrating device signals the need for embrace and support.
The Social Roots of Resistance to Seeking Help
The \good mother\ myth is like an invisible shackle. One mother of two candidly admitted: admitting to being depressed feels like admitting to parenting failure. This social expectation leads 59% of afflicted mothers to choose silence. There’s a silver lining, though, as more celebrities and public figures begin to share their experiences, which has increased hotline consultation numbers by 35%.
The innovative practices in the business sector deserve attention. One internet company provides psychological transition leave for new parents, allowing staggered returns to work paired with professional consultations. This institutional support more effectively addresses practical problems than merely extending maternity leave.
Map of Co-Response Strategies for Couples

Key Indicators for Symptom Recognition
Pay attention to these three warning signs: emotional numbness lasting more than two weeks, sudden loss of interest in previous hobbies, and the emergence of somatic symptoms (such as unexplained pain). Early detection is more important than perfect responses. It is recommended to set up phone reminders for a simple weekly self-assessment using the PHQ-9 scale.
Innovative Dialogue Mechanism Establishment
Emotion weather stations serve as a practical tool: each day, describe your mood using weather symbols (sunny/cloudy/thunderstorm), and partners adjust their interactions based on the weather report. This method reduces the pressure of directly discussing emotions, making 86% of trial couples report smoother communication.
Collaborative Self-Care Plans
- Set up a charging station: designate a relaxation area in the living room.
- Exchange free time vouchers: give each other 2 hours of alone time each week.
- Create a sensory first-aid kit: prepare soothing oils, stress relief toys, etc.
Practice shows that co-designed self-care plans have a 73% implementation rate. It is crucial to translate abstract concepts into specific, actionable items.
Integration and Utilization of Professional Resources
When selecting a therapist, it's advisable to prioritize experts with a background in family systems therapy. A clinic in Beijing's three-person consulting model (couple + therapist) has yielded significant effects, with 89% of participants reporting improved mutual understanding.
Wisely Constructing Support Networks
The operational model of the online community Firefly Alliance is worthy of reference: groups sorted by children’s age, matching partner families with similar experiences. This precise support has increased the efficiency of seeking help by 40%. At the same time, it’s recommended to cautiously filter information sources and beware of absolute advice found online.
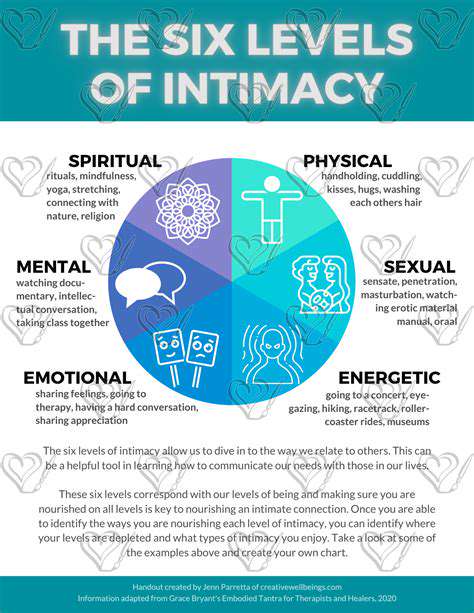
Resilient Redefinition of Intimate Relationships
Try a new definition of intimacy: view accomplishing parenting tasks together as a cooperative achievement rather than merely a division of responsibilities. Some couples have invented an achievement badge system, adding a commemorative symbol each time they successfully cope with a challenge, and this gamification design has rekindled intimacy for 73% of participants.
Timing for Professional Interventions

Accurate Identification of Warning Signals
When persistent insomnia is accompanied by mood swings that are heavier in the morning and lighter at night, or if there are thoughts of harming oneself or the baby, immediate professional help must be sought. Data from a crisis intervention center in Shanghai shows that timely help can reduce the incidence of dangerous behaviors by 82%.
Precise Connection to Medical Resources
It is recommended to familiarize oneself with local mental health resources and create an emergency contact card. A three-color grading assessment system from a community hospital in Beijing is worth promoting: it matches different levels of intervention measures based on the severity of symptoms.
Skills Training for Partner Involvement
Participate in supporter workshops organized by the hospital to learn practical skills such as effective accompaniment during appointments and recording symptom changes. Data shows that trained partners can improve treatment collaboration by 65%.
Innovative Models of Social Support
- Extend corporate EAP plans to postpartum care.
- Establish parent stations in communities for new parents.
- Develop AI emotional companion robots to assist in monitoring.
A tech company’s smart wristband project in Hangzhou predicts depression risk by monitoring heart rate variability and sleep patterns, with an accuracy rate of 79%.
Reasonable Expectations for the Recovery Process
Use a quarterly assessment method: evaluate progress every three months across emotional, cognitive, and behavioral dimensions. Remember, recovery is not a straight path, but a spiral upward. Allow for setbacks and focus on long-term trends.
Scientific Combination of Integrative Therapies
Combine mindfulness meditation with dance therapy to create a unique mind-body synchrony therapy. Research shows that this combination can enhance emotional regulation abilities by 43%. At the same time, note that herbal treatments should be conducted under professional medical guidance.
Stage-based Self-Reconstruction Strategies
Follow three steps: survival mode (ensuring basic routines) - recovery mode (rebuilding interests) - growth mode (developing new skills). Set specific achievable goals for each stage, such as completing three 10-minute walks this week.
Read more about Postpartum Depression’s Effect on Marriage and Recovery Tips
Hot Recommendations
- Multigenerational Home Living Arrangements and Marriage Strain
- Surrogacy Legal Guidance for Same Sex Married Couples
- Steps to Repair Broken Trust When Marriage Feels Fragile
- Montessori Parenting Styles and Their Impact on Marital Unity
- Sensate Focus Exercises Recommended by Sex Therapists
- “I Statement” Formulas to Express Needs Without Blame
- Tiny House Living Adjustments for Minimalist Married Pairs
- Highly Sensitive Person (HSP) Marriage Dynamics and Coping
- Post Traumatic Growth Strategies for Crisis Surviving Marriages
- Daily Gratitude Practices to Boost Marital Appreciation