Aging Parent Caregiving Duties and Marriage Preservation Tips
Index
Providing care encompasses assisting with daily needs, coordinating medications, and preserving self-respect.
The strain of caregiving can test marital bonds; maintaining dialogue proves indispensable.
Defined expectations and collaborative task management boost care effectiveness and relational harmony.
Scheduled check-ins create role transparency for families navigating care obligations.
Difficult dialogues arise naturally; handle them with compassion and focused attention.
Attentive hearing holds equal weight to verbal exchange in care-related communication.
Expert mediation can ease complex discussions surrounding elder care challenges.
Sustaining connections remains paramount when juggling care commitments.
Personal limits safeguard against exhaustion while improving care provider fulfillment.
Strategic scheduling enhances caregiver self-renewal practices.
Support networks reduce care burdens and offer psychological reinforcement.
Joint engagements reinforce partnerships amid care obligations.
Local programs enable collective experiences for couples and relatives.
Acknowledging excessive strain proves critical; honest family dialogue provides relief.
Investigate assistance programs and temporary relief options to mitigate caregiver pressure.
Continual evaluation of caregiving's marital effects remains essential.
Navigating Care Obligations
Core Care Components
Supporting aging relatives involves multifaceted duties that reshape family interactions. Assistance with personal hygiene routines - bathing, dressing, and grooming - often demands substantial commitment, particularly when mobility limitations exist. These acts of care, while time-intensive, form the bedrock of preserving self-respect and physical comfort.
Medication oversight represents another vital responsibility. Organizational strategies like compartmentalized pill cases or Medication Management applications prove invaluable. Research indicates approximately four in ten older adults misuse prescriptions, potentially exacerbating health conditions. Consistent monitoring and reminder systems help maintain proper treatment adherence.
Relationship Preservation Strategies
Maintaining romantic connections while caregiving requires intentional effort. The emotional toll of Caregiving Responsibilities frequently strains partnerships, with time constraints and fatigue sparking disputes. Proactive dialogue prevents misinterpretations, while deliberately reserving couple time sustains emotional bonds despite external pressures.
Implementing role clarity through mutual agreements often reduces overwhelm. Studies reveal that divided responsibilities not only enhance operational efficiency but also deepen emotional intimacy. This cooperative model serves dual purposes - optimizing care delivery while nourishing the partnership foundation.
Dialogue Dynamics in Care Contexts
Caregiving Realities
Approximately 18 million Americans provide unpaid elder care, creating complex relational dynamics requiring nuanced communication. Clear conversations establish role parameters, preventing misunderstandings that might erode care quality or family cohesion.
Optimizing Information Flow
Families benefit from implementing structured communication systems - weekly check-ins, shared digital calendars, or dedicated messaging threads. Research confirms that organized communication correlates with higher satisfaction and reduced tension among care teams. Platforms like CareZone centralize updates, freeing mental space for quality care provision.
Navigating Sensitive Topics
Essential yet uncomfortable discussions regarding health directives or financial planning demand tactful handling. Creating psychological safety through non-judgmental listening often yields better outcomes than directive approaches. Validation techniques help surface unspoken concerns needing attention.
The Listening Imperative
Effective care communication balances information exchange with absorption. Care providers who master reflective listening techniques often achieve deeper understanding of both practical needs and emotional undercurrents. This dual focus builds trust - the cornerstone of sustainable care relationships.
Expert Consultation Benefits
Neutral third-party facilitators like geriatric care managers often break communication deadlocks. These professionals help families confront challenging realities while maintaining relational harmony. Medical providers can clarify treatment protocols, aligning family expectations with clinical requirements.
Relationship Nourishment Tactics
Balancing care obligations with partnership health demands creativity. Scheduled connection rituals - morning coffee talks or weekly walks - help maintain intimacy. Transparent emotional check-ins foster mutual understanding, while collaborative problem-solving reinforces team dynamics.
Boundary Setting for Sustainable Care
The Boundary Advantage
Demarcating personal limits prevents role engulfment, with studies showing boundary-aware caregivers experience 23% lower burnout rates. Explicitly communicating availability windows and task capacities helps families align expectations, reducing friction.
Temporal Optimization
The Eisenhower Matrix helps prioritize urgent/important tasks, while batch-processing routine activities boosts efficiency. Surprisingly, care recipients often value engaged presence over task completion speed - a 15-minute quality conversation can sometimes outweigh hours of physical care.
Boundary Articulation Techniques
Effective Communication is Paramount when establishing limits. Phrasing like I can assist with morning routines but need afternoons for work commitments sets clear parameters. Quarterly family summits allow boundary adjustments as care needs evolve.
Replenishment Practices
Neuroscience research reveals that brief daily mindfulness sessions (as short as 12 minutes) significantly lower caregiver stress markers. Caregivers Who Engage in Self-Care report 40% higher relationship satisfaction. Micro-breaks - gardening or journaling - serve as effective pressure valves.
Support Infrastructure
Local Area Agencies on Aging offer sliding-scale respite care, while platforms like Care.com connect families with vetted helpers. Peer support networks provide both practical tips and emotional validation, reducing isolation.
Reinforcing Partnerships Through Shared Experiences

Interest Alignment Process
Rekindling connection begins with inventorying current passions versus nostalgic interests. Shared Activities might blend individual hobbies - perhaps combining photography walks with nature journaling.
Novelty Seeking
Brain scan studies show novel activities activate dopamine pathways similarly to early romance. Monthly adventure dates trying new cuisine or geocaching can revive relationship vitality. Many communities offer couple-focused workshops from blacksmithing to mixology.
Time Protection Strategies
- Block calendar slots for connection activities
- Implement no care talk zones during couple time
- Create ritualized check-ins (Sunday breakfast reviews)
Protected time segments prevent caregiving from monopolizing the relational space. Even 20-minute daily debriefs help maintain emotional synchronization.
Intergenerational Engagement
Multigenerational cooking sessions or family history projects create shared meaning. Involving care recipients in modified activities (adapted gardening, memory scrapbooking) fosters inclusion while easing the care dynamic.
Community Utilization
Local museums often host adult-friendly nights, while parks departments offer guided nature walks. These low-cost options provide structured interaction opportunities without extensive planning.
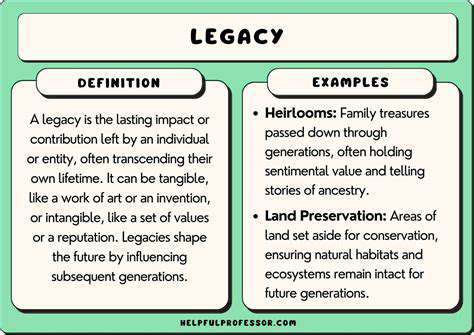
Collaborative Visioning
Jointly planning a future garden renovation or vacation creates forward-focused energy. Common Goal pursuit activates teamwork neural pathways, enhancing partnership cohesion. Celebrating micro-milestones (saving 25% for a trip) maintains motivational momentum.
Identifying Support Intervention Points
Stress Indicators
Prolonged sleep disturbances or emotional numbness often signal excessive strain. Feelings of Overwhelm lasting over two weeks warrant intervention. Cortisol level testing sometimes objectively confirms burnout states.
Capability Assessment
Honest self-evaluation checklists help gauge capacity limits. The Modified Caregiver Strain Index provides validated metrics for determining assistance needs. Consistently missing personal appointments often indicates role imbalance.
Resource Mapping
Medicare-covered respite programs offer 4-8 hours weekly relief in many regions. Faith-based organizations frequently provide volunteer companionship services. Hybrid support models blending professional and community resources often prove most sustainable.
Family Recalibration
Structured negotiation techniques help redistribute tasks. Using a task board with sticky notes allows visual workload distribution. Some families implement rotating primary caregiver months to share responsibility equitably.
Marital Impact Tracking
Monthly relationship audits using Gottman Institute tools help quantify caregiving's partnership effects. Scheduled getaways (even local staycations) provide crucial perspective shifts. Couples reporting decreased conflict after implementing caregiving-free evenings.
Professional Intervention Timing
When daily functioning becomes impaired or health declines emerge, geriatric care managers (average cost $125-$200/hour) create customized care plans. Many Employee Assistance Programs offer free counseling sessions for working caregivers.
Read more about Aging Parent Caregiving Duties and Marriage Preservation Tips
Hot Recommendations
- Multigenerational Home Living Arrangements and Marriage Strain
- Surrogacy Legal Guidance for Same Sex Married Couples
- Steps to Repair Broken Trust When Marriage Feels Fragile
- Montessori Parenting Styles and Their Impact on Marital Unity
- Sensate Focus Exercises Recommended by Sex Therapists
- “I Statement” Formulas to Express Needs Without Blame
- Tiny House Living Adjustments for Minimalist Married Pairs
- Highly Sensitive Person (HSP) Marriage Dynamics and Coping
- Post Traumatic Growth Strategies for Crisis Surviving Marriages
- Daily Gratitude Practices to Boost Marital Appreciation